Both Google and Microsoft are investing heavily in
PHRs. The companies had senior-level managers at the
Health Care IT Summit in San Diego, Nov. 2008. The event was engineered by
The Everything Channel.
Grad Conn is Microsoft’s Senior Director of Global Consumer Health Strategy in the Health Solutions Group.
Alfred Spector’s Google title is Vice President of Research and Special Initiatives. PHRs are one of those special initiatives, apparently.
The two IT giants approach PHRs differently.
Microsoft launched HealthVault in October 2007. It’s a PHR platform designed to store and access personal health and fitness information. It combines single HealthVault records—the storage piece (with access provided by Windows Live ID) —with Live Search Health, a search engine that allows HealthVault users to search for health and fitness information. HealthVault accomodates both the
CCR and
CCD standards, the latter of which was approved in 2007, and whose proponents say essentially harmonize with
HL7s CDAs with CCRs.
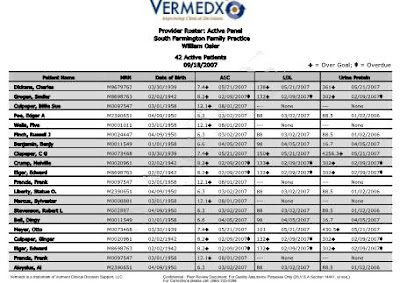
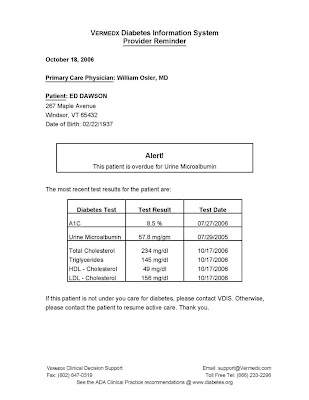
Google Health is a PHR in which users voluntarily enter their health records and create one, centralized profile. Even though Google maintains it will not sell advertisin in Google Health, privacy concerns have dogged the concept since it was unveiled in May this year. Google is partnered with Walgreens, CVS, Quest Diagnostics (also a
Vermedx® partner), Beth Israel Deaconess Medical Center, and other entities.
Its application programming interface is based on the CCR—an XML-based standard for health records developed to allow physicians to create and transfer electronic health records with ease. “We have no intention of [involving advertising]
at this juncture,” said Google’s Spector. (The emphasis is mine.)
Spector explained that one of Google’s key motivations is “. . . the epidemiological research value in the data. It must somehow be valuable over the long term, where we knew drug ‘x’ affected person ‘y’ because of a certain set of factors, and that [a person] could check for not just correlation but cause and effect. Down the road I think that’d be an incredible contribution to the world.”
In contrast, HealthVault is a software and services platform. Conn explained that "like PayPal, we’re an intermediary." Microsoft’s Ballmer has been quoted as saying that health care is one of the top six bets the company is making.
The personal nature of health records, the understanding required to interpret them correctly, and the obvious need for security and privacy have been highhurdles for designers of health data systems. But it appears the design phase is nearly complete, and roll-out is beginning.